Minister Butler announced $7.8 million in funding for public awareness and workforce training to support hepatitis B elimination. Frank Carlus, Vice President of Hepatitis Australia, emphasised the urgency of sustained investment, aiming to meet the 2030 goal of eradication. Currently, there are nearly 300,000 Australians live with hepatitis B or C, risking severe liver disease.
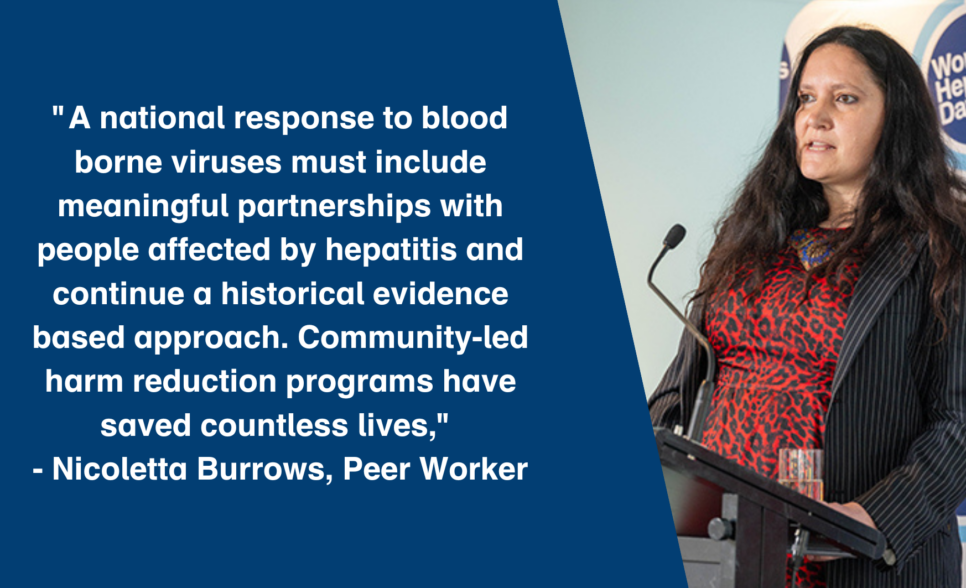
Community voices, including Nicoletta, who stressed the importance of community-led responses and partnerships to drive effective strategies .
Transcript from Nicoletta’s inspiring speech:
Before I begin, I would like to extend my thanks to Selina Walker for her generous welcome to country/acknowledgment of country, and to acknowledge the lands we stand on today are the traditional and unceded lands of the Ngunnawal people.
I am a peer community development worker- and like all peer workers, I wear several hats simultaneously.. I am speaking as an employed peer worker, as a person who has lived experience of hepatitis c- as an active – and unapologetic- injecting drug user, an unrepentant sex worker, and as an advocate for my community – a community that has been on the frontlines of the hepatitis c epidemic.
My involvement in community development work exceeds 2 decades and upholds a robust tradition of peer-instigated harm reduction practice.
Over the past 20 years, I have seen many changes in how viral hepatitis has impacted my community. There have been some incredible and much-needed changes, namely, low threshold access to DAAs to treat hep c; dedicated hepatitis a and b vaccination programs; and increased recognition of the expertise that peers bring to the sector workforce.
However, I have also seen the dilution of evidence-based responses to blood-borne virus prevention for the sake of populism and political opportunism, and I am keenly aware of the frustration that many in my community feel at what seems like a lack of progress in responding to the preventable deaths, unnecessary suffering, and systemic stigma and discrimination many of us continue to experience.
Communities of injecting drug users continue to be most impacted by hepatitis c, and despite decades of work, we are still advocating for systemic reforms that would significantly alleviate the harms we experience– to name the elephant in the room, I am referring to tough-on-drug policies. As demonstrated by the recently introduced NSW’s Mandatory Testing Orders, policy is regressing.
The hysterical underpinnings of mandatory testing orders are at odds with Australia’s largely evidenced-based response to blood-borne viruses.
Australia’s pragmatic harm reduction response has historically been led by the expertise of affected communities. Injecting drug users, sex workers, and the LGBTIQ community have been at the fore of these efforts and through meaningful partnerships between State and community, Australia has continued to curb a potentially more devastating viral hepatitis epidemic.
Peer advocates, community development workers, and activists have been integral to this process, and our work has been undertaken despite the compounding impacts of criminalisation, stigma and discrimination, and historically poor treatment options.
Peer workers are not just a unique asset to the viral hep response, we are essential to its success.
However, our work is often stymied by a lack of resources and the impacts of criminalisation.
In considering strategies to end hepatitis, we recognise that treatment is only part of the solution. Whilst biomedical responses inevitably save many lives- they must be complemented by meaningful investment in community responses that utilise peer-led health promotion and community development principles. These responses must be underpinned by a harm-reduction approach.
Similarly, ending viral hepatitis must involve recognition and acknowledgment of the impacts of legislation on our communities. There are decades of evidence that highlights how the carceral system and the criminalisation of people who use drugs exacerbate blood-borne virus transmission. Drug law reform is not just urgently overdue, it is an essential component of a holistic response to end viral hep.
Finally- given the theme of World Hep Day 2024, I encourage you all to consider what taking action to end viral hepatitis means.. Communities of people affected by hep c need you to be fearless in your approach – many of the people in this room have powerful platforms that could be utilised to enact meaningful action..
For example..
For the sector workforce, I urge you to draw on the experiences of peer workers. Peer workers are highly skilled and knowledgeable, and can engage our communities in meaningful and creative ways. If your service or organisation doesn’t have any peer workers – I urge you to ask why not and to be proactive in creating avenues for meaningful peer participation. If your service only has peers as volunteers or only employs a “palatable” peer, I encourage you to question why you are not engaging peers from diverse class, ethnic, and living experience backgrounds.
To the media- People living with blood-borne viruses are not vectors of disease, nor are we fodder for a sensationalist soundbite. Consider your reporting of viral hepatitis and how you frame socio-political issues that directly impact people affected by hepatitis. Does your reporting reflect nuance or do you merely contribute to stale tropes that exacerbate stigma and discrimination? Do you platform the voices of people directly affected by the issues you are reporting on? If not, why not?
To the policymakers here today- communities impacted by viral hepatitis are not merely a priority population- we are diverse and varied individuals who make significant contributions to the spaces we exist in. When you are pondering your next policy position paper or key recommendations for the minister- I urge you to consider creating space for meaningful community consultations, led by people who will be directly impacted by the policies you are tasked with drafting. Listen to what we are telling you, even if what we say is uncomfortable for you to hear. We experience significant harm from how policy and legislation are implemented, and our survival often involves making unenviable choices in navigating policies you drafted.
And lastly, to our esteemed elected representatives here today- you, better than most know that with great power comes great responsibility – consider whether legislation you propose and endorse addresses the social determinants of health (and ultimately uplifts our entire society), or whether it will exacerbate harms against already marginalised people. I urge you to be courageous and reject populism – use your position to create a legacy of change by working with our communities, not against us.
Draw on the historical approaches used in early blood-borne virus strategies. Commit to responses that are developed and implemented in meaningful partnership with people affected by viral hepatitis.
Appropriately resource our representative organisations. Be fearless in supporting evidence-based policy change..And remember – the decisions you make directly impact our lives.
Thank you.